
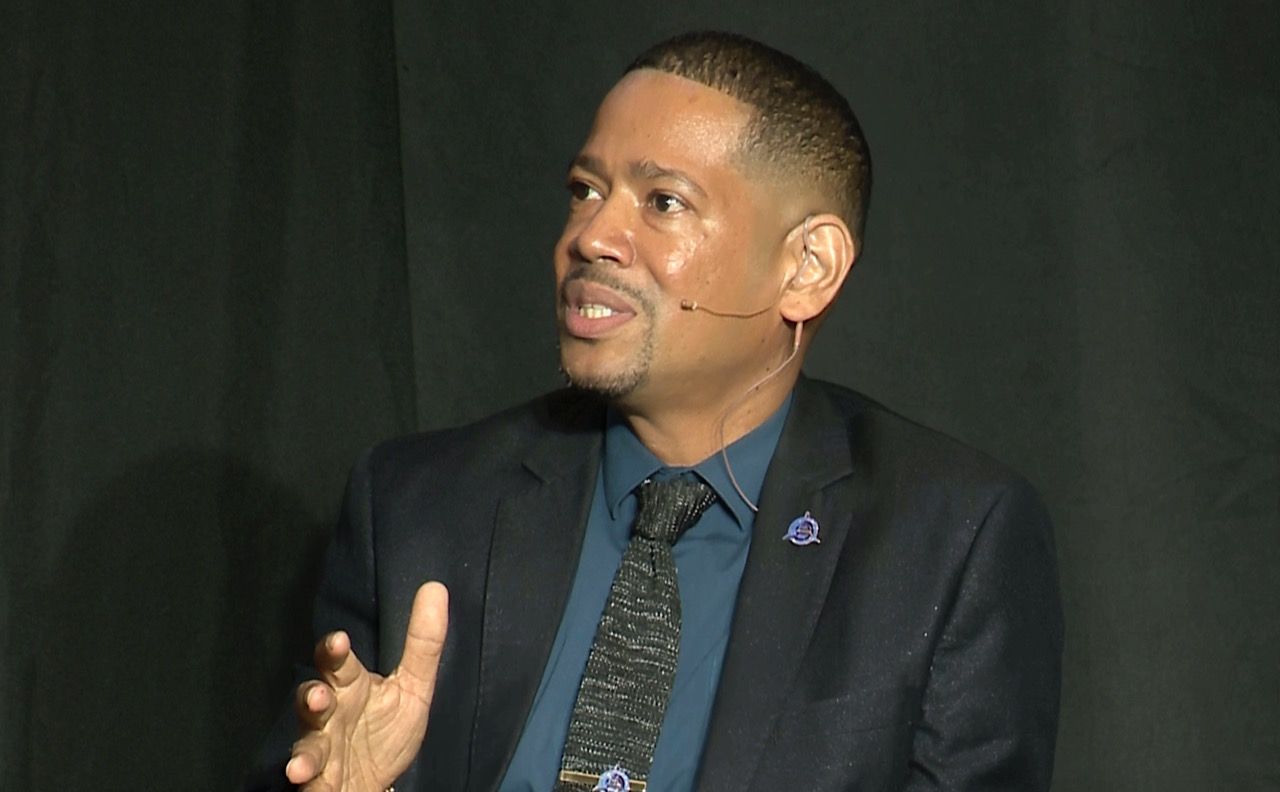
Above: Dr Navi Muradali speaking at the panel discussion. Photos by Mark Lyndersay.
BitDepth#1462 for June 10, 2024
A small group of medical professionals gathered at the Dalai Lama space at One Woodbrook Place on May 26 to discuss the state of digital health solutions.
Leading the panel discussion was Dr Navi Muradali of Patient Connect, which is dedicated to the concept of digital health technologies.
During covid lockdowns Muradali enabled telehealth sessions, eventually having discussions with 9,000 patients in partnership with SEWATT and the Supermarkets Association.
Of that number, the vast majority, some 80 per cent, sought mental health counselling, another ten per cent were general practitioner (GP) consultations while the remainder were counselled by dieticians and other care services.
“I wouldn’t be able to say what percentage of persons proceeded to an in-person session as we do not keep records after the telehealth sessions ended,” Murdali explained in response to questions emailed after the event.
The Virtual Wellness telehealth sessions essentially cratered after covid restrictions were lifted.
Jamaica has continued using telehealth, confirming that e-prescriptions are legal in the country in June 2022. They are not in TT.
Muradali acknowledged the value of in-person consultations in this change locally.
“People who were using telehealth were happy to go back to their in-person doctors for that personal touch,” he said.
“Telehealth should never replace in-person care but should support patients and doctors and mental health counsellors with hybrid care. Patient Connect is working on easy to use hybrid care systems such as chat-based care allowing the use of chat bots and humans to provide easily [and continuously] accessible care.”
“In Trinidad and Tobago, we are defined by a two-tier health system, public and private, many people do not go to the public simply because you have to spend the day,” said Ava Rampersad, CEO of the Family Planning Association.
“In the public health system, most clinics right now on a Sunday afternoon it’s closed and you may have to go to a hospital and you would then have to wait all day. If it’s a particular clinic like a diabetic clinic; for example, you have to go between Monday to Friday. So it means then that they have to take a day off work, which means they may not be able to go.”
The other option is private healthcare, which is cost prohibitive, so many people try to find a happy medium. And so they look for solutions that convenient and accessible.”
“I think that with the accountable and responsible use of AI – it doesn’t have to be the fanciest thing since sliced bread – but it can be simple solutions that enhance the experience for the patients, or the clients using a hybrid approach with face to face that helps the service experience.”
With interest diminishing in telehealth, the Virtual Wellness project evolved into Patient Connect, which champions app and AI driven solutions as a way to deliver low cost health and wellness services and related resources.
One success had been the adoption by the Human Resource Management Association, which has implemented a Wellness Hub powered by Patient Connect’s technology that’s still onboarding clients and marketing its services.
The emphasis is on business to business opportunities and the company is in discussions about using its technology with other clients.
Patient Connect is developing a privately built and assessed dataset resource for chatbots and AI search to offer a more reliable alternative to “Dr Google” and using AI to deliver systems that assist practitioners in delivering services and virtual connectivity solutions that enable digital connections with patients to improve preliminary diagnosis.
The planned systems will address primarily wellness services, routine preventative care and some urgent care.
One issue that Patient Connect hopes to address is the problem of patient self-diagnosis via search engine.
“I’ve had instances where we have clients who would have gone to other pharmacies in other areas and received prescriptive medication without prescription,” said Rampersad.
“So this person would have been self-treating for something that is not properly diagnosed and obviously the situation will escalate. By the time they get to our doors, the medical situation would have gotten to the point where first line treatment might not necessarily work.”
“I see misinformation when clients actually believe influencers on Facebook, Tiktok and Instagram [that] one or two mindful therapy sessions will quickly fix their stresses and anxiety,” said psychologist Anu Bissessar.
“That’s not true. People believe [that by] meditating once or twice that they can be cured right away. There’s no quick fix to chronic anxiety and pressure.”
“Yes, you can get relief in a short time frame by doing these temporary exercises, but to make a great impact and change your brain chemistry from anxious to calm, you definitely need to implement these techniques every day.”
“Young people these days don’t have the time, or they don’t want to take the time to actually sit with their thoughts.”
In developing its own OMNI artificial intelligence agent, Patient Connect is training the large language model locally on selected resources, including information from NGOs and care providers.
The development team is reviewing how the AI accesses this information to ensure that it is both easy to use and accurate when it accesses information that’s both geographically and culturally informed by the Caribbean experience.
Muradali remains wary of the capacity of AI systems to hallucinate, making up facts with great authority.
Patient Connect also hopes to be involved in the introduction of Electronic Medical Records (EMR) and Electronic Health Records (EHR) to Trinidad and Tobago and the wider Caribbean.
Like many technologies that promised a relief from the burdens of paper-based records, EMRs and EHRs have quickly gained a reputation as being burdensome to maintain and update.
Globally, Muradali said, doctors are wary because, “Instead of talking to my patients, I have to be typing.”
EMRs are used by medical professionals to manage patient cases while EHRs are meant to be a portable digital record of a patient’s medical profile that can quickly establish baselines for a new care provider.
“EHR systems in the local public hospitals have been reported to be a bit difficult for staff to use, buggy, and may not be interoperable,” Muradali explained.
“The private sector has various EHR’s in use, but no system is easily integrated when patients have to get records sent to another nursing home. Epic, which is the largest EHR [system] in the USA, is now being integrated with AI-medical scribes to reduce the burnout doctors and nurses have been experiencing because of cumbersome and time-consuming EHRs.”
“Patient Connect has been reviewing EHR systems across the world and working on an AI-assisted EMR. Nowhere in the Caribbean has an all-in-one EHR connecting public and private health sectors.”
While the discussions were wide-ranging in the panel discussion, Muradali hopes that the attendees, largely comprised of medical professionals, would, “become more comfortable with digital health technologies and AI in healthcare.”
“We need to get to the point that public and private healthcare workers both appreciate digital health education and literacy as the building blocks [for change].”






































[…] Trinidad and Tobago – A small group of medical professionals gathered at the Dalai Lama space at One Woodbrook Place on May 26 to discuss the state of digital health solutions… more […]